Treatment of Rhinocerebral Mucormycosis
A Successful Treatment of Rhinocerebral Mucormycosis involving Maxilla and Salvage Surgery by Dr. Mathan Mohan
INTRODUCTION
Mucormycosis is a rare and potentially lethal, invasive fungal infection caused by any of several related molds of the Mucoraceae family. This fungus is often found in decaying organic matter including spoiled bread, fruit, and vegetables, as well as soil and compost piles.
This fungal infection causes fatal form of rhinocerabral mucormycosis. It is a rare opportunistic infection of the sinuses, nasal passages, oral cavity, and brain. Rhinocerebral mucormycosis commonly affects individuals with diabetes and those in immunocompromised states such as hemochromatosis, malignancy, or those who undergo organ transplantation, severe burns, trauma and prolonged corticosteroid therapy. When the disease involves the orbit, it becomes fatal and increases the chance of mortality and morbidity to the patient.
Symptoms of rhinocerebral mucormycosis include:
- Swelling on one side of the face
- Headache
- Nasal or sinus congestion
- Fever, pain, and sometimes cough.
- Black lesions on nasal bridge or upper inside of mouth
CASE REPORTS
We are presenting a series of 2 cases with known diabetes who were only treated with medical management elsewhere with a 1-month course of Amphotericin B and other antifungals.
The first case was 55 year-old diabetic male patient typically presenting as headache, especially in parietal and frontal lobes, accompanied by a discharge from the nose.
The second was 48 year-old diabetic male patient typically presenting localised pain in maxilla.

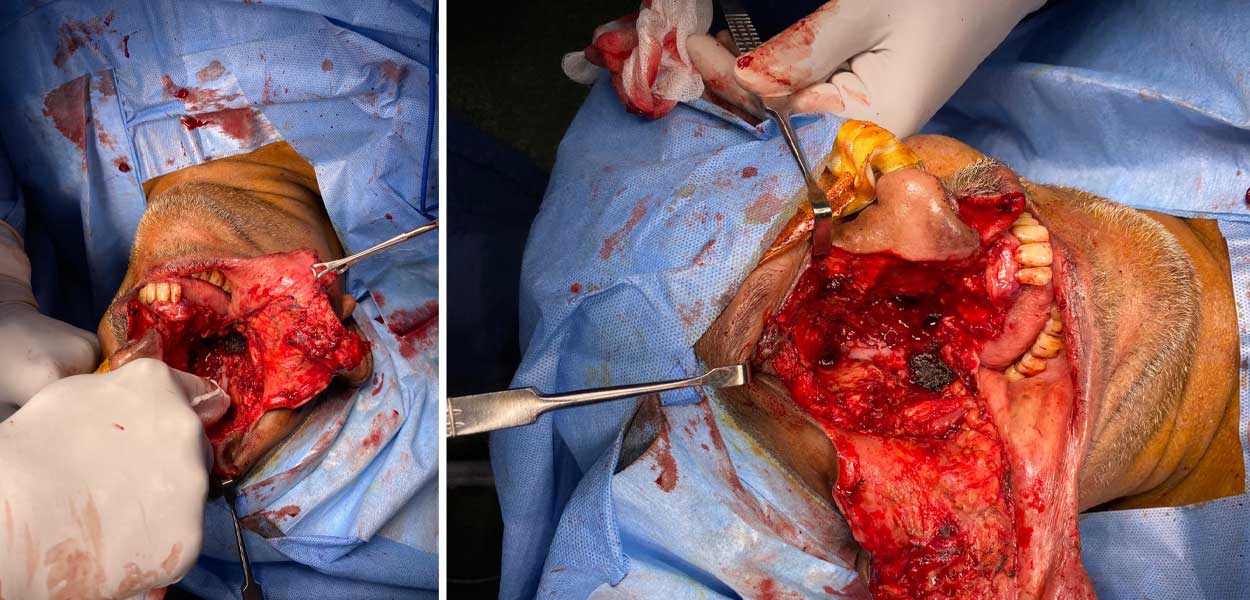
After extensive clinical and laboratory examination of both the cases, Dr. Mathan nominated both for maxilla and salvage surgery. MRI and CT Scan demonstrated soft tissue lesions in diagnosis of cavernous sinus thrombosis. The results showed that the orbit was invaded. The infection began in the paranasal sinuses and progressed to the orbit. An increased density of the orbital fat was seen in both the patients.
The surgery assured the eradication of the disease and the patients were released from hospital. The patients were followed up for 6 months and were free of the disease.
CONCLUSION
Dr. Mathan, Head and Neck Surgical Oncologist, emphasizes the importance of early detection and correction of underlying systemic condition with radical surgery in the management of this fatal disease.
ACKNOWLEDGEMENT
Dr Mathan appreciates the team that collaborated with him in this surgery.